

Serious adverse reactions occurred in 26% of patients. In Checkmate 205 and 039, adverse reactions leading to discontinuation occurred in 7% and dose delays due to adverse reactions occurred in 34% of patients (n=266). The most frequent serious adverse reactions reported in ≥2% of patients were acute kidney injury, pleural effusion, pneumonia, diarrhea, and hypercalcemia. In Checkmate 025, serious adverse reactions occurred in 47% of patients receiving OPDIVO (n=406). Fatal intestinal perforations occurred in 3 (0.9%) patients.
The most frequent serious adverse reactions reported in ≥2% of patients were diarrhea, pneumonia, pneumonitis, pulmonary embolism, urinary tract infection, and hyponatremia. In Checkmate 9ER, serious adverse reactions occurred in 48% of patients receiving OPDIVO and cabozantinib (n=320). The most frequent serious adverse reactions reported in ≥2% of patients were diarrhea, pyrexia, pneumonia, pneumonitis, hypophysitis, acute kidney injury, dyspnea, adrenal insufficiency, and colitis.
#CHECKMATE 9LA BRAIN METASTASES PLUS#
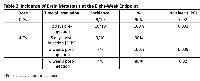
In Checkmate 214, serious adverse reactions occurred in 59% of patients receiving OPDIVO plus YERVOY (n=547). Fatal adverse reactions occurred in 4 (1.3%) patients and included pneumonitis, acute heart failure, sepsis, and encephalitis. The most frequent serious adverse reactions reported in ≥2% of patients were pneumonia, pyrexia, diarrhea, pneumonitis, pleural effusion, dyspnea, acute kidney injury, infusion-related reaction, musculoskeletal pain, and pulmonary embolism. In Checkmate 743, serious adverse reactions occurred in 54% of patients receiving OPDIVO plus YERVOY. In Checkmate 057, fatal adverse reactions occurred these included events of infection (7 patients, including one case of Pneumocystis jirovecii pneumonia), pulmonary embolism (4 patients), and limbic encephalitis (1 patient). The most frequent serious adverse reactions reported in ≥2% of patients receiving OPDIVO were pneumonia, pulmonary embolism, dyspnea, pyrexia, pleural effusion, pneumonitis, and respiratory failure. In Checkmate 017 and 057, serious adverse reactions occurred in 46% of patients receiving OPDIVO (n=418). Fatal adverse reactions occurred in 7 (2%) patients, and included hepatic toxicity, acute renal failure, sepsis, pneumonitis, diarrhea with hypokalemia, and massive hemoptysis in the setting of thrombocytopenia. The most frequent (>2%) serious adverse reactions were pneumonia, diarrhea, febrile neutropenia, anemia, acute kidney injury, musculoskeletal pain, dyspnea, pneumonitis, and respiratory failure. In Checkmate 9LA, serious adverse reactions occurred in 57% of patients (n=358). Fatal adverse reactions occurred in 1.7% of patients these included events of pneumonitis (4 patients), myocarditis, acute kidney injury, shock, hyperglycemia, multi-system organ failure, and renal failure. The most frequent (≥2%) serious adverse reactions were pneumonia, diarrhea/colitis, pneumonitis, hepatitis, pulmonary embolism, adrenal insufficiency, and hypophysitis. In Checkmate 227, serious adverse reactions occurred in 58% of patients (n=576). No fatal adverse reactions occurred in patients who received OPDIVO in combination with platinum-doublet chemotherapy. Now it can be said that with this regimen their survival is similar to patients without brain metastases.Dual immunotherapy-based combination resulted in clinical benefits across key subgroups of mNSCLC patients with high unmet need, including those with PD-L1 expression 2% included pneumonia and vomiting. He concludes by saying the results from this study can at the very least give hope to patients with brain metastases found at the time of diagnosis, whereas, previously mentioned, they had a terrible prognosis. He says that patients with brain metastases at base-line who were treated with Chemo alone did quite poorly, whereas the patients treated with IPI + NIVO + Chemo did just as well as patients without brain metastases. This study was randomised, so 51 patients were in the NIVO + IPI + Chemo arm, and 50 were in the Chemo only arm. He begins by recapping on how 30 years ago brain metastases were a truly horrible prognosis with a 6 week median survival after diagnosis.ĭr Carbone then goes onto explain that they identified 101 patients that had brain metastases at base-line. Dr David Carbone talks to ecancer about the results from CheckMate 9LA: First-line nivolumab (NIVO) + ipilimumab (IPI) + chemo in patients with advanced NSCLC and brain metastases.


 0 kommentar(er)
0 kommentar(er)
